Professor creates innovative training tool to help surgeons save new mothers’ lives

Esther Chin, Global Health lead in the department of Obstetrics & Gynecology, has developed STITCH, a portable, affordable, reusable simulator that allows clinicians to practise treating postpartum hemorrhage, a complication that kills tens of thousands of women each year.
BY Beth Gallagher
October 22, 2024
Esther Chin always planned to become a neurosurgeon or a cardiac surgeon. Then she spent time in a small, remote hospital nestled in the mountains of Rwanda.
“I saw pregnant women hike for ten hours while fully dilated,” says Chin, “I saw moms and babies die.”
The experience moved Chin to change her career plans.
Today, she is the Global Health lead in McMaster’s department of Obstetrics & Gynecology, and the founder of a new venture called STITCH — Surgical Trainer for Interventions to Control Postpartum Hemorrhage.
The STITCH team has developed a simulator for health-care providers to practise important procedures to stop excessive bleeding after a birth — a complication that still results in thousands of deaths every year.
Chin, whose grandmother was an obstetrician in Myanmar, says STITCH is part of her goal of bringing safe surgical care to marginalized communities around the world.
“I am using a health equity lens and perspective, coupled with innovation, to mobilize change,” says Chin. “We’re all very excited to get STITCH into the hands of people who need it most, to impact the 14 million people who experience postpartum hemorrhage every year, and the 70,000 preventable deaths each year.”
Surgical simulators: Like flight simulators for pilots
The aviation industry has used flight simulators for decades to ensure that pilot trainees are ready to respond to an emergency, Chin points out. The same principle applies to health-care providers, who need practise to be able to respond to a medical emergency, especially in remote or underserviced communities.
“It’s possible that learners could go through training and not encounter any of these cases. Then they’re on-call as an independent practitioner and a patient has a postpartum hemorrhage that is not responding to medical treatment, thereby requiring these surgical procedures,” says Chin.
“You don’t have the luxury of time to look things up or call someone, if there is surgical backup in that setting,” says Chin. “You have to act.”
Chin, who completed a master’s degree in Global Surgical Care at the University of British Columbia, developed STITCH with students in its Master of Biomedical Engineering program — Noah Stewart, Tara Kemper, Vincent Levandier, Yiting Wu and Yong Hui Chan.
Three surgical procedures that save lives
There are other simulator models on the market, but they are large and heavy, which makes them unwieldy and drives up shipping and labour costs, especially in rural or remote communities and low- and middle-income countries.
STITCH is designed to be portable, reusable and affordable, she says, to improve access for end users around the world.
It fits into a carry-on suitcase and is far less expensive than the $10,000-$15,000 high-fidelity simulators currently on the market.
The base of STITCH is based on an MRI of a female pelvis, making it more realistic than the homemade textile models in simulating the true breadth and depth of the surgical field.
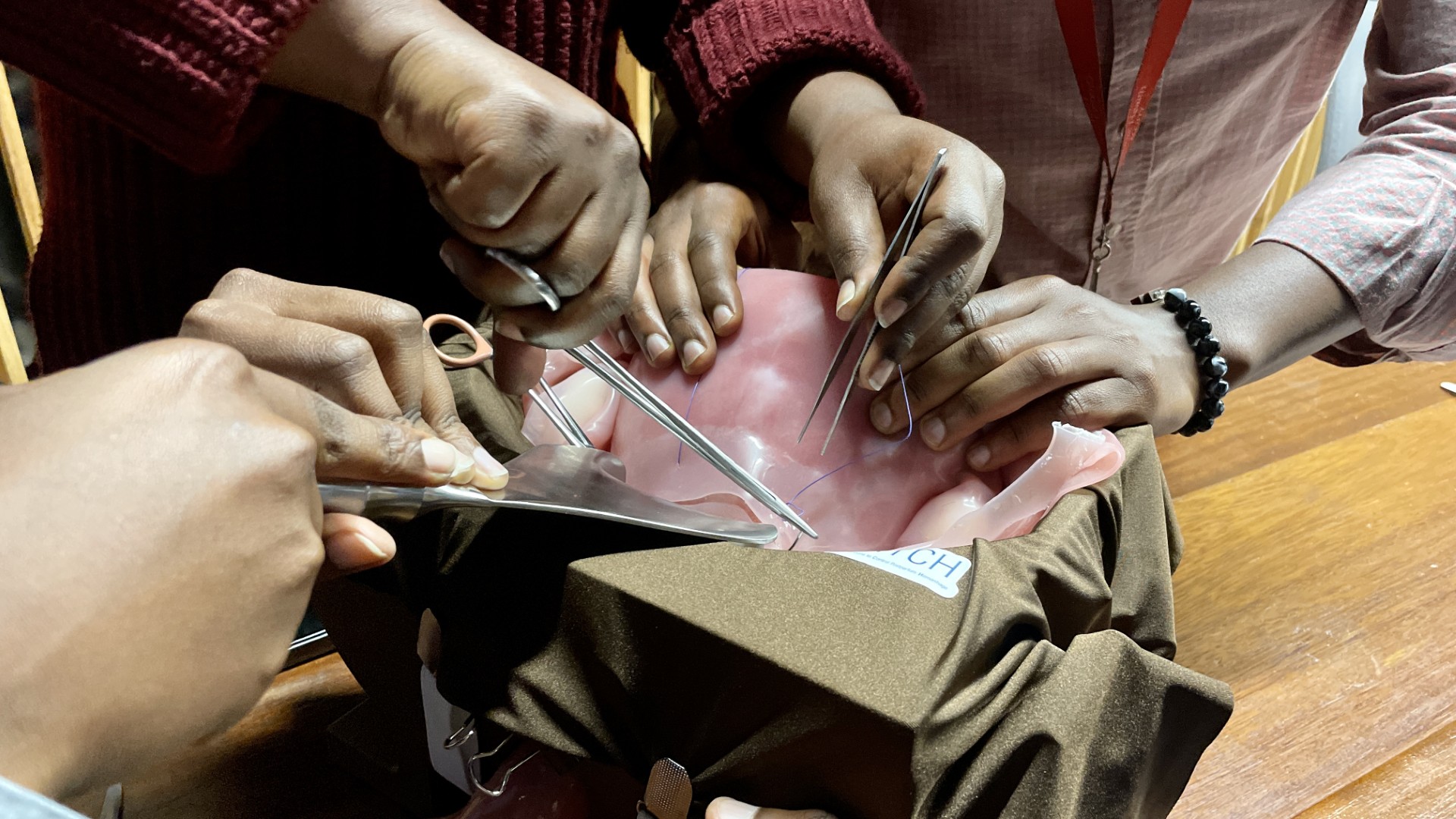
The STITCH simulator helps health-care providers practise three critical procedures when faced with catastrophic bleeding after a birth:
- Compression sutures: A surgical stitch that controls bleeding by applying direct pressure to the uterus.
- Tying arteries: A procedure that involves tying off the arteries to the uterus to stop the main blood supply.
- Hysterectomy: The removal of the uterus is the last-resort effort to save the life of the patient.
STITCH was showcased at the Society of Obstetricians and Gynecologists of Canada Annual Clinical and Scientific Conference in June.
Chin also presented STITCH at the Rwanda Society of Obstetricians and Gynecologists Annual Scientific Conference in Kigali, Rwanda in September.
STITCH is manufactured in Vancouver, but the long-term plan is to shift manufacturing to sub-Saharan Africa to supply end users in the region, support local industry, improve sustainability and reduce the carbon footprint.
Chin is also applying for a grant to build a curriculum around the simulator, and connecting with end users around the world for validation studies.


