Analysis: COVID-19 vaccine inequity allowed Omicron to emerge

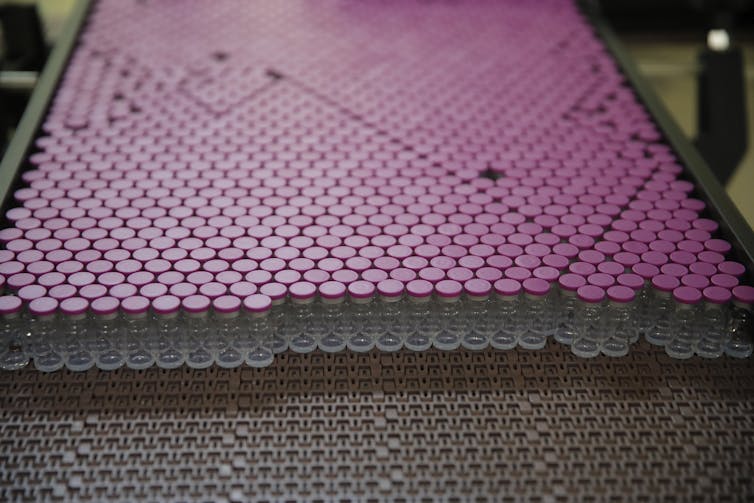
While people in the wealthy West have had preferred access to multiple rounds of vaccines, vast numbers of people, especially in Africa and on the Indian subcontinent, haven’t received a single dose.(Pixabay/Canva)
BY Dawn Bowdish and Chandrima Chakraborty
December 14, 2021
Canada’s COVID-19 vaccination rate is 76 per cent — 10 times higher than it is across the continent of Africa.
While people in the wealthy West have had preferred access to multiple rounds of vaccines, vast numbers of people, especially in Africa and on the Indian subcontinent, haven’t received a single dose. This has permitted the virus to thrive and accelerated the process of mutation, adding months and perhaps years to the pandemic.
Wherever COVID-19 has the chance to linger, variants develop and travel. This entirely predictable pattern is destined to repeat itself unless countries with resources share vaccines with others that cannot afford them.
Wealthy countries have yet to meet their pledges to provide equitable global access to vaccines via COVAX (an international collaboration to procure and distribute COVID-19 vaccines) and other initiatives. The resulting lack of broad global vaccine coverage made the rise of another variant like Omicron inevitable.
For Canada, it is more critical than ever to carefully balance the supply of vaccines available for domestic use while prioritizing international sharing — and encouraging regional manufacturing.
Millions of pre-ordered vaccine doses
When the COVID-19 crisis started, major manufacturers pre-sold their vaccines to governments as they were being developed but before they were tested, as a way of funding their work, including clinical trials.
Canada and other developed countries ordered millions of doses, enough to cover their populations many times over, with promises to share their excess vaccines with other countries. That has not happened quickly enough. While logistical, legal and other barriers did impede the wider distribution of vaccines, there appears to be a lack of will to overcome them.
The momentum gained by accelerating the development of vaccinations has now been lost.
Third doses and booster shots will be important to controlling both the ongoing threat of Delta and the spread of Omicron. Canadians should certainly heed public health guidance and get their shots when they are recommended. Once vaccine doses are in Canadian freezers and fridges they aren’t going anywhere, and declining a dose won’t mean that it is redistributed to other parts of the world that need them.
On a federal level, Canada should only buy what is needed domestically and commit to accelerating the distribution of vaccines elsewhere. The same is true for all wealthy countries.
The rise of Omicron
Watching the rise of Omicron is particularly frustrating. It has been apparent since the outset that the spread of COVID-19 needed to be slowed globally, precisely to prevent variants from emerging. That message should have been clearer after the spread of the agile Alpha variant. It should have been clearer still from the swift attack of the Delta variant.
Variants like Delta and Omicron will arise when the burden of infection is high and vaccination rates are low, as is the case with many countries in the Global South. Identifying variants by their country of origin perpetuates a long legacy of representing racialized people as originators or carriers of disease.

In fact, the world has been served well by South Africa’s admirable investments in disease surveillance that turned up the newest COVID-19 threat.
There is no way to know where in the world the Omicron variant actually emerged, even though it was first detected in South Africa. South Africa has been down this road before with HIV, and had a well-developed pandemic surveillance system that allowed it to detect this variant.
Investing in global health
Canada has not historically invested in global health, infectious disease research or in vaccine innovation and manufacturing.

As a result, our country is a consumer of COVID-19 vaccines rather than a contributor to the global supply. Despite having small manufacturing facilities that had capacity to contribute a few million doses, Canada lacked the political will to repurpose these facilities to assist with the global vaccine effort.
Regional manufacturing here and abroad could enable quicker worldwide vaccination. Vaccine manufacturers are already contracting local manufacturers in India and Africa to make vaccine doses, but these doses are being shipped to the West instead of being available locally. Sharing knowledge and technology that can help countries in the Global South develop vaccines and vaccinate their own populations will have a greater long-term benefit for the world than trying to stop variants by closing borders.
As the crisis has worn on, we have invested in domestic manufacturing in Canada, but it will take years to staff these plants with trained personnel, let alone create innovative vaccines that are more suitable for distribution to the Global South.
Rather than being consumers who contribute to inequitable vaccine distribution, we have an opportunity to weave vaccine equity into these investments.
We can commit to training people from countries where vaccines are needed most to equalize access to expertise. We can commit to global partnerships to distribute manufacturing equitably and we can be advocates for change.
As we rebuild and invest in vaccine development and production, we have an opportunity to become leaders in vaccine equity and reduce the burden of infectious disease now and in the future.
Do you have a question about COVID-19 vaccines? Email us at ca-vaccination@theconversation.com and vaccine experts will answer questions in upcoming articles.![]()
Dawn ME Bowdish, Canada Research Chair in Aging & Immunity, McMaster University and Chandrima Chakraborty, Professor, English and Cultural Studies; Director, Centre for Peace Studies, McMaster University. This article is republished from The Conversation under a Creative Commons license. Read the original article.


