Hamilton patient first to receive experimental immunotherapy for cancer
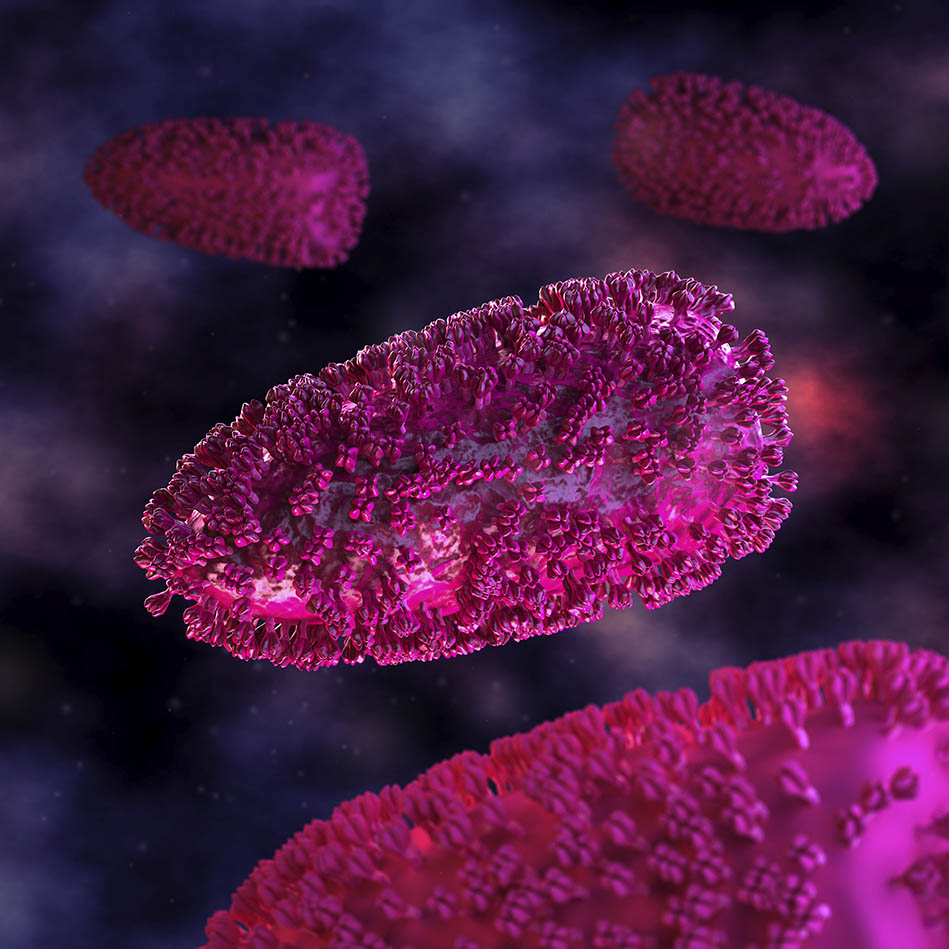
The experimental MG1MA3 virus used in this trial is derived from a virus called Maraba that was first isolated from Brazilian sandflies. It has been engineered to infect and kill cancer cells directly, while also triggering an immune response against the cancer cells.
May 1, 2017
A Hamilton patient is the first trial participant to receive a novel experimental immunotherapy treatment for lung cancer.
Experts at Hamilton Health Sciences (HHS) and McMaster University, in partnership with The Ottawa Hospital, have begun a clinical trial to determine if the unique experimental immunotherapy combination may be able to treat non-small cell lung cancer. The experimental therapy combines two different viruses with an approved drug to stimulate the immune system to recognize and attack cancer cells.
“Lung cancer is the most common kind of cancer in Canada, with more than 28,000 new diagnoses each year,” said trial leader Dr. Rosalyn Juergens, oncologist at HHS and associate professor of oncology at McMaster. “We’ve come a long way in improving our patients’ survival rates and outcomes, but we can do more. Immunotherapy is the leading edge of a new wave of cancer treatment – we’re excited about the potential that it offers to patients with this devastating disease.”
The first patient enrolled in the “Sandpiper” trial was recently treated at Hamilton Health Sciences’ Juravinski Hospital and Cancer Centre. An additional 54 patients are expected to be enrolled in the trial and treated in Hamilton and Ottawa, as well as other sites.
“In recent years, immunotherapy has shown great promise in treating certain kinds of cancer, but we’re still at the early stages of understanding and optimizing this approach.” said Dr. Garth Nicholas, medical oncologist and trial leader at The Ottawa Hospital, and assistant professor at the University of Ottawa. “We hope that this new combination of immunotherapies will make a difference for people with lung cancer.”
The viral therapy being tested is called MG1-MAGEA3 and uses two engineered viruses that were jointly developed by Dr. Brian Lichty (McMaster University), Dr. David Stojdl (Children’s Hospital of Eastern Ontario, University of Ottawa), and Dr. John Bell (The Ottawa Hospital, University of Ottawa), and their respective research teams and colleagues.
The two viruses used are MG1MA3, which is derived from a virus called Maraba that was first isolated from Brazilian sandflies, and AdMA3, which is derived from a common cold virus called adenovirus. Both of these viruses have been engineered to stimulate an immune response against cancer cells that express a protein called MAGE-A3. The Maraba virus also achieves an extra layer of anti-cancer activity by replicating inside many kinds of cancer cells and killing them directly.
The trial combines these two viruses with a drug called pembrolizumab, which Health Canada approved for the treatment of cancer in 2016. Pembrolizumab stimulates an immune response against cancer cells by targeting a protein called PD-1.
This trial is primarily funded and sponsored by Turnstone Biologics, a company co-founded by Drs. Lichty, Bell and Stojdl. Turnstone also made an announcement about the trial launch today. Additional funding partners include BioCanRx and the Ontario Institute for Cancer Research.
Many organizations have supported the research that led to this trial, including The Ottawa Hospital Foundation, CHEO Foundation, Ontario Institute for Cancer Research, Canadian Cancer Society, Terry Fox Research Institute, Canadian Institutes of Health Research, Ministry of Research, Innovation and Science, Canada Foundation for Innovation, Ottawa Regional Cancer Foundation, Hair Donation Ottawa, Angels of Hope, BioCanRx, Pancreatic Cancer Canada, NAV Canada and several philanthropic donors.


