Program with community volunteers promising in reducing health-care use by older adults
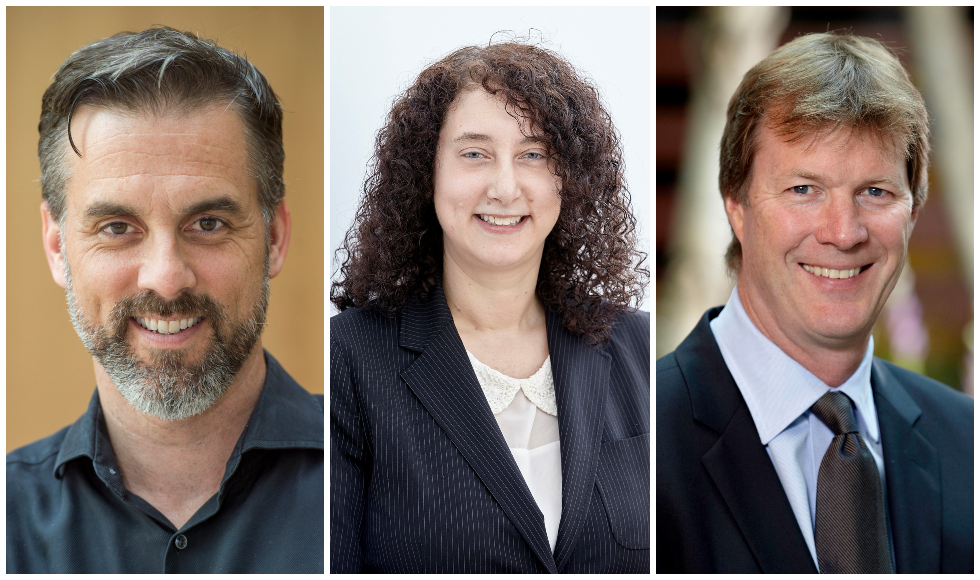
From left: Doug Oliver, Lisa Dolovich and David Price of McMaster's Department of Family Medicine.
May 6, 2019
Incorporating community volunteers into the health-care system shows promise in reducing health-care usage by older adults through a shift from hospitals to primary care, according to research from McMaster.
Results of the Health TAPESTRY (Health Teams Advancing Patient Experience: Strengthening Quality) project were published today in the Canadian Medical Association Journal (CMAJ).
“We found that older adults who took part in the Health TAPESTRY program changed the way in which they used health-care services,” said Lisa Dolovich, lead author and professor in the Department of Family Medicine at McMaster. “Encouragingly, participants had more visits to primary care with fewer emergency department and hospital admissions compared to those not in the program.”
Health TAPESTRY is a community-based program anchored in primary care where trained volunteers visit older adults in their home. Volunteers use technology to gather information on their goals, needs, and risks, and a summary is sent to interprofessional primary care teams to plan patient care. The program combines new elements like technology with the current health system to support optimal aging in adults aged 70 years or older.
Doug Oliver, co-author and associate professor in the Department of Family Medicine said: “Health TAPESTRY leverages the enormous resource of community volunteers and integrates them into the formal primary health care system. The volunteers give health care teams access to information they might not have otherwise known, which means they can offer more proactive, person-centered care.”
While results from the randomized controlled trial did not affect the primary goal of the study, which was to help older adults to reach their health goals, there were other positive effects experienced by the intervention group compared to the control group.
For example, there was an increase of 81 minutes of weekly walking time in the intervention group compared with a 120-minute decrease in the control group, and the intervention group reported higher overall levels of physical activity. The volunteers gave primary health-care teams information that the health providers might not have otherwise known.
David Price, co-author, and professor and chair of the Department of Family Medicine, said: “These findings suggest that Health TAPESTRY has the potential to improve the way primary care is delivered in Canada by shifting care of individuals away from hospitals to the community and to a more proactive and preventative team-based model of care.”
Read the paper here.
Learn more about Health TAPESTRY here.


