Candida auris: What’s known about the rapid spread of the drug resistant fungus
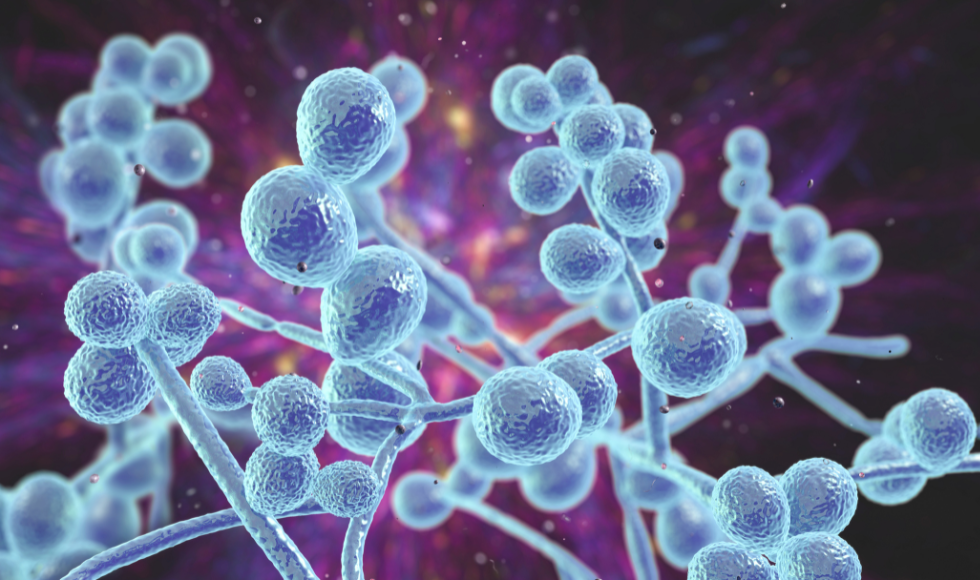
Candida auris is an emerging fungus that is resistant to multiple antifungal drugs commonly used to treat Candida infections. (Shutterstock)
BY Maureen Lawlor
March 31, 2023
Candida auris (C. auris), an emerging fungus and serious global health threat, spread at an “alarming rate” in U.S. health care centres throughout 2020 and 2021, according to the Centers for Disease and Control Prevention (CDC).
The fungus can be difficult to identify, spreads easily and can cause severe and sometimes lethal bloodstream infections, particularly among those with serious medical problems.

It’s resistant to multiple antifungal drugs, and its spread could have serious implications for the Canadian health care system, according to the Public Health Agency of Canada.
Jianping Xu, a professor in the Department of Biology and Faculty of Science Research Chair in Understanding Fungal Threats to Humans, helped lead the first team of researchers to isolate C. auris in a natural environment.
Xu, who is also a researcher with Canada’s Global Nexus for Pandemics and Biological Threats, shares what researchers know about the fungus and how it may be spreading so quickly.
What do we know about the emergence of C. auris?
This fungus was first recognized as a distinct species in 2009 by a Japanese scientist who recovered the yeast from the ear of a patient. Since then, it has been recorded in over 50 countries, where it’s caused primarily hospital-related outbreaks and also common infections. After its sudden emergence, researchers began analyzing samples taken before 2009 to see if they had been misidentified to other species. And indeed, they identified samples that also had this fungal infection. The first current known live culture is from the mid-1990s.
Where are we finding C. auris?
So far, we have been primarily finding it in hospital environments causing nosocomial [health care-acquired] infections. And it can persist in a hospital environment for extended periods of time. Some of the strains are resistant to disinfectants, to dryness — whatever stress you put on them. And this fungus can also grow at high temperatures, for instance at 42 degrees, which is well above our typical fever. It’s also quite resistant to osmotic stress — those high saline and other types of environments that are typically stressful for organisms. This fungus is just somehow able to fend it off and survive and thrive in those environments.
We really don’t know much about the entire transmission route, but it’s most likely it’s through contact. We know we shed. For instance, if it’s in the ear wax and we shed the ear wax, it could be released into the environment. It’s been found in all kinds of environments in hospitals — the bedding, the pillows, the sinks, the floors. Once they are there, it’s quite resistant to some of the disinfectants we use to mop them off. And when a new person or another person comes in, they can pick it up.
Tell us about the drug resistant nature of C. auris
Most of the strains are drug resistant and resistant to multiple drugs. Almost all of them are resistant to fluconazole, which has been one of the major drugs for treating candida infections like the typical yeast infection. And a high proportion are also resistant to the other types of drugs like polyenes and Flucytosine.
A recommended line of treatment has been Echinocandins, which have been effective for the last 13 or 14 years, although now if you read recent U.S. reports, they have found drug resistant strains against this drug as well.
Resistance to all the currently applied antifungal drugs, as well as previously applied antifungal drugs have been reported in other fungi. But typically, each of those resistant strains is only resistant to one or a couple of related drugs, not to the whole spectrum. So, this is quite unique for C. auris.
Right now, the specific mechanisms are not really well understood, but one of the hypotheses is that because of C. auris’ ability to handle the high temperature and high stress that led to some of the emergence of the fungus in the first place — those features also enable them to be resistant to some of those drug-induced stressors.
What do scientists think prompted its sudden emergence?
When we have genetically divergent lineages of the same species that emerged at very similar times at different parts of the world, it suggests some kind of common denominator. Arturo Casadevall and his colleagues at Johns Hopkins University have proposed that global warming may be responsible. We are seeing the temperature increase in certain parts of the world and fungal stressors building up. There’s also increased human movement and the potential for bringing environmental microorganisms to the human environment.
Thanks to your work, we know C. auris can also be found in the natural environment. Tell us more about that.
Until a couple of years ago, all the isolates were obtained from patients, or from hospital environments. And then two years ago, with colleagues in India and here at McMaster, we analyzed salt marsh islands from the Andaman Islands in the Bay of Bengal in the Indian Ocean — a very hot and humid environment with high osmotic pressure. And we found natural strains of this species. So that was the first report of the fungus in a natural environment.
Then last year, again with colleagues in India, we looked at stored apples as a potential source. For many stored fruits we use fungicides to extend their shelf life and storage life, and the wax layer we coat on them has some compounds similar to our ear wax. So, we wanted to look at whether stored apples could be a source. And indeed, we found genetically different strains of C. auris.
What we think is that the ecological niche itself — the stored apple with the wax coating — can become a selective force for growth of the fungus. There are nutrients there — they can utilize and digest the wax, as well as other compounds. And the fungicide would probably kill off others, allowing the more resistant strains of fungi like C. auris to colonize. And once they colonize, it becomes a selective environment in that they could become more and more resistant, and the mutations that allow them to be more resistant would survive in that environment. And then, stored apples are supplied to many parts of the world year-round so that could potentially lead to spread.
What’s next for researchers studying C. auris?
Scientists are now looking at the samples that have been submitted for metagenome sequencing — samples from soil, fresh water, salt water, air samples, human samples. And indeed, we are now finding more and more signatures of this fungus in those kind of environments. No live culture has been found yet in animals, but I think it’s only a matter of time that we’re going to find those kind of connections.


