High-intensity interval training could help women battle breast cancer

January 19, 2018
McMaster scientists have found that high-intensity interval training – commonly known as HIIT – boosts both the number and activity of “natural killer” cells in overweight and obese women with breast cancer.
Natural killer cells are a type of white blood cell that is important in eliminating tumours and virally infected cells.
These results come on the heels of previous research that reported similar results in normal weight females.
Results of the study were published in the Journal of Cancer Prevention.
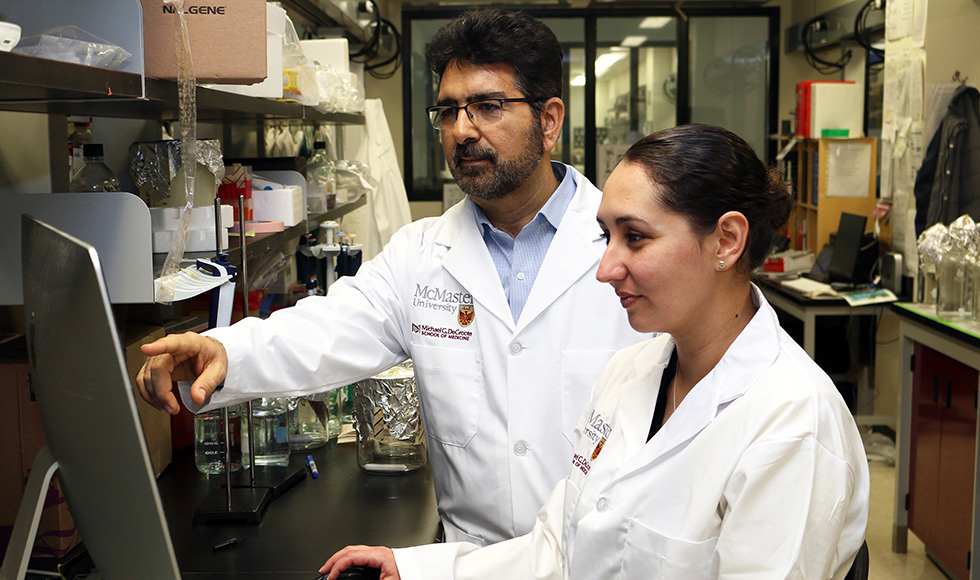
“While we knew the impact of HIIT on normal weight subjects, whether it had the same impact in overweight and obese women was not well established,” said Ali Ashkar, study author, professor in the Department of Pathology and Molecular Medicine at McMaster and the McMaster Immunology Research Centre.
Ashkar also holds the Tier 1 Canada Research Chair in Natural Immunity and Natural Killer Cell Function.
“Our results in obese mice challenged with breast cancer suggest that HIIT is a promising therapeutic option that may translate to normal, overweight, and obese human breast cancer patients.”
Obesity is a risk factor for many illnesses, including breast cancer in women. In pre- and post-menopausal breast cancer patients, obesity is associated with a noticeable reduction in survival compared to normal weight patients.
Research suggests that the increased risk of death is caused by impaired innate immunity, or a reduced natural ability for the body to fight off disease.
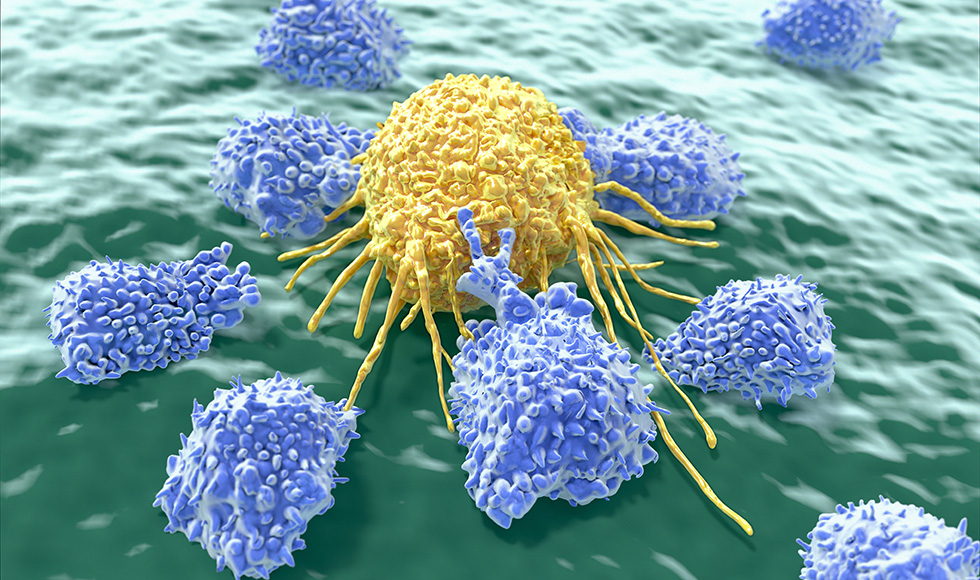
Natural killer cells are responsive to exercise. HIIT, in particular, results in a greater increase in the number and function of natural killer cells than moderate intensity exercise.
McMaster researchers based their study on outcomes in mice, as well as in three overweight and obese women.
“The circulating natural killer cell number and activation markedly increased immediately after HIIT,” said Nicole Barra, first author and postdoctoral fellow at McMaster. “It also enhanced metabolic health and reduced tumour burden, which refers to the size of a tumour.”
Additional authors on the study are from McMaster’s Department of Pathology and Molecular Medicine and McMaster Immunology Research Centre, the Michael G. DeGroote Institute for Infectious Diseases Research, the Department of Kinesiology, Department of Medicine, and the Department of Biochemistry and Biomedical Sciences.
The study was supported in part by funding from the Canadian Institutes of Health Research.


